As the novel coronavirus COVID-19 continues to spread across the country, our teams are finding new ways to use The Power of FoodTM to comfort and nourish patients and caregivers. This journey has led us to share best practices that can help guide healthcare foodservice operations.
This information is the cumulation of experience and research from some of the industry’s leading healthcare practitioners.
As part of our efforts, we have pulled together recommendations that can guide changes in healthcare foodservice to ensure the safety of your teams. These practices are broken into two categories: Pandemic Plan and Pop-up Hospitals.
Pandemic Plan
A pandemic differs from usual types of emergencies in that the entire country is involved, as with the novel coronavirus COVID-19. The “enemy” itself – the virus – is invisible, but the effects are not.
When the novel coronavirus was declared a pandemic, Morrison Healthcare and Compass One Healthcare implemented our corporate pandemic plan throughout our different accounts. Our teams have found this plan to be valuable because it gives them access to a wide range of resources. Multiple heads are better than one when thinking through scenarios, and our on-site directors can take the plan and run with it.
A feature that is especially convenient for directors is the multi-approach pandemic menu, which has already been entered into the production system. This allows the director to implement it when the need arises.
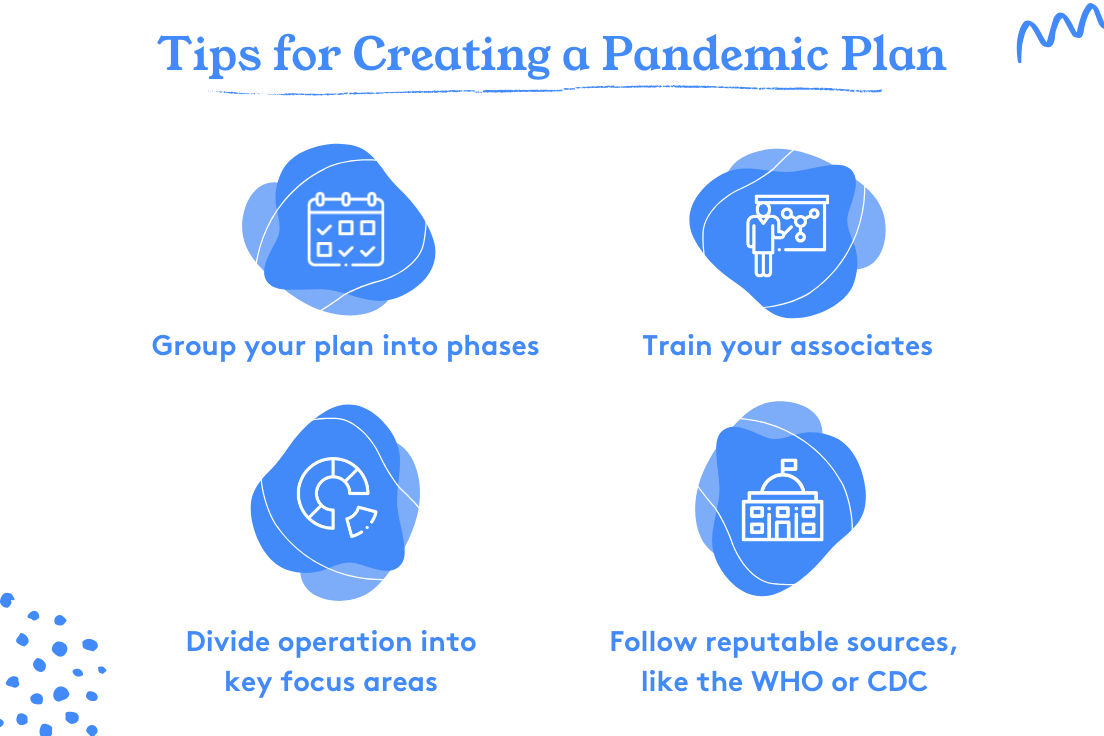
While the best time to prepare for a pandemic is before it happens, there are a few best practices you can follow if you want to modify your response or consider additions to the plan you already have in place.
Here are some lessons we have learned from this pandemic:
- Group your plan in phases. You can use our structure as a guide:
- Planning Phase
- Prepare plan
- Train
- Practice Phase
- Practice drills to ensure readiness
- Early Response Phase (complete when an outbreak is in the US and looks to be heading towards a pandemic)
- Reinforce proper food safety and personal hygiene policies
- Ensure all information in the planning phase is accurate and ready to use
- Response Phase
- Outline steps to follow in the event of a pandemic
- Utilize resources from credible sources such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC)
- Implement guides on what resources to use and where to find them
- Follow government directives
- Train your associates and practice your plan.
- Look at your operation and divide it into focus areas. We split ours into communication, purchasing, operations, HR, and IT.
- Always follow reputable sources for information such as the CDC and WHO.
Pop-up Hospitals: Healthcare Foodservice in Alternative Locations
As the novel coronavirus COVID-19 continues to spread, American institutions are opening pop-up hospitals to relieve overcrowded hospitals.
Morrison Healthcare, along with its parent company Compass One Healthcare, has developed a guide to support the opening of pop-up hospitals, and ensure the strictest safety protocols and seamless foodservice operations.
To design this new process, our team had to take into consideration the limitations these pop-up sites can present. The equipment available might not be the same as we are used to in a regular hospital, the design of the room could be different, and there may be limited staff or foodservice staff who are not accustomed to working in acute care environments.
We understood that a simple menu and process would be the best to execute in these pop-up hospitals since the set up would not be what we were accustomed to. Basic, easy to understand, and repeatable were vital in the design of the menus and playbooks we developed for pop-up hospitals.
To help guide similar operations, we are sharing best practices we’ve observed and lessons we’ve learned in the field.
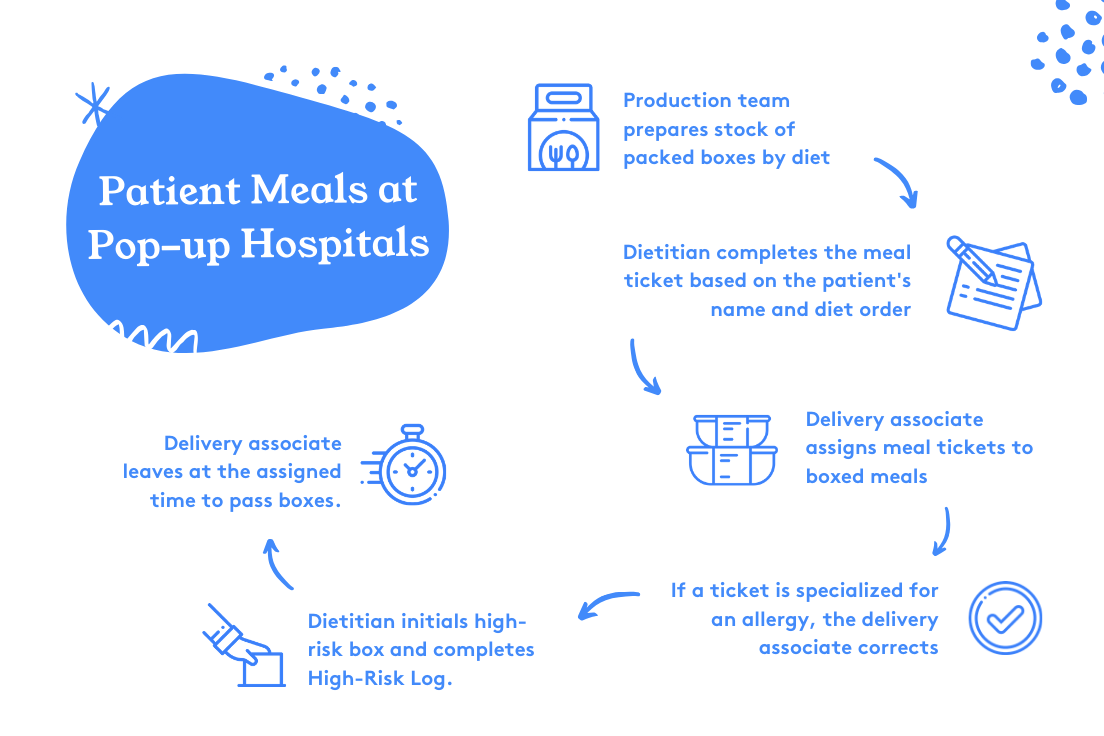
Basic Process
Patient meals destined for pop-up hospitals are prepared by the culinary team and packaged in boxes by diet for easy distribution. A registered dietitian should always be on-site to ensure meal tickets are completed with the patient’s name and diet order.
If a patient has a food allergy, the delivery associate should customize the meal to ensure that the allergen is removed and safe for the patient. The dietitian should double-check the patient’s meal while initialing and completing a high-risk log. The associate then delivers the patients’ meals at the appropriate and assigned times.
Avoiding Adverse Effects
To prevent any adverse effect, use a High-Risk Meal Check Log at each meal. This will capture and monitor all patients with a food allergy and/or food texture/liquid thickness prescription. A dietitian or supervisor should obtain a report from the electronic medical record system that lists the patients with food allergies and food texture/liquid thickness.
The report must be printed less than an hour before the start of the meal assembly to ensure you include new patients. It should also be modified after printing by writing in the names of any patients with new orders for food allergies and/or food texture/liquid thickness.
High-Risk Meal Delivery
Add a red sticker to the ticket to identify high-risk trays.
Meal Distribution by Nursing
At some pop-up hospitals, nursing may be delivering the boxed meals to the patients. In this instance, we suggest having designated tables representing each diet, so the nurse can pick up and distribute them to the patient.
If you’d like to read more about what Morrison Healthcare has been doing to combat the novel coronavirus COVID-19 and best practices, visit our Resource Center.